What Code Set Describes Medical Necessity
CPT codes are an integral part of the billing process used by insurance companies in healthcare. Coders take medical reports from doctors which may include a patients condition the doctors diagnosis a prescription and whatever procedures the doctor or healthcare provider performed on the patient and turn that into a set of codes which make up a crucial part of the medical claim.

Hcpcs Codes Hcpcs Level Ii Coding Aapc
Per the CMS Internet Only Manual IOM Medicare Claims Processing Manual Publication 100-04 Chapter 12 Section 3061 A Medical necessity of a service is the overarching criterion for payment in addition to the individual requirements of a CPT code.

. CPT code 88175 88155 88164 88165 88150 - Cervical Cytology Value Set Procedure code and Description 88175 Cytopathology cervical or vaginal. CPT codes are used to describe tests surgeries evaluations and any other medical procedures performed by a healthcare provider on a patient. C Describes the restrictions on the disclosure of the employees medical information the employer representatives or other parties with whom the information will be shared and the methods that the covered entity will use to ensure that medical information is not improperly disclosed including whether it complies with the measures set forth in the HIPAA regulations.
Choose the code that best describes the method. Since both methods of EEG monitoring would not be utilized in the same 24-hour period the two procedures are mutually exclusive of one another. Medical Necessity listed in the LCD.
For EM services medical necessity of a visit as well as the CPT level of the service must both be documented. Title XVIII of the Social Security Act section 1862 a1A. This section excludes coverage and payment for items and services that are not considered reasonable and necessary for the diagnosis and treatment of illness or injury or to improve the function of a malformed body member.
The medical record should reflect two total testosterone and free testosterone levels when indicated to determine the medical necessity of testosterone replacement. For certain items and services medical necessity and coverage are established through a prior authorization PA process. Providers are reminded to code to the highest level of specificity with a diagnosis to support medical necessity when submitting.
FAQ about Medical Billing CPT CODE 96372. Medical necessity has not been met for billing speech therapy. CPT code 95953 describes monitoring by computerized portable electroencephalography 16 or more channel EEG and CPT code 95956 describes monitoring by cable or radio 16 or more channel telemetry.
A diagnosis of onychomycosis can allow 11720 or 11721 if it has either a Q modifier but does not need a MD or DO last seen or if it has one of the 6 ICD-9 codes listed in the special section for onychomycosis ie. If medical necessity is not met the insurance company will deny the claim. Medical coding is a little bit like translation.
The Current Procedural Terminology CPT code for diagnostic dilation and curettage DC is 58120. NON-MEDICAL NECESSITY COVERAGE AND PAYMENT RULES For any item to be covered by Medicare it must 1 be eligible for a defined Medicare benefit category 2 be reasonable and necessary for the diagnosis or treatment of illness or injury or to improve the functioning of a malformed body member and 3 meet all other applicable Medicare statutory. The following example describes an EM service that is separately identifiable from a therapeutic and diagnostic Injection.
B For most covered items and services medical necessity has already been established and is simply confirmed on a case-by-case basis through the completion of a CMN when applicable. All services rendered must be met by medical necessity and have the appropriate ICD-10-CM diagnosis code. This denial reason code is received when a procedure code is billed with an incompatible diagnosis for payment purposes and the ICD-10 codes submitted isare not covered under an LCD or NCD.
Medical necessity assures services are reasonable and necessary for the diagnosis or treatment of illnessinjury. It is an exception to the application of Subsection b of Section 17822 or Section 17823 of this code that a person describes or labels food as kosher-style and if the description is written the words kosher and style are of the same size type or script. Difficulty with walking 68110 68111 7030 7197 7295 7812.
/color-therapy-definition-types-techniques-and-efficacy-5194910_final1-972d594f507449908c885a41347a4a1d.png)
Color Therapy Definition Types Techniques Efficacy

Fee Schedules The Method Of Choice For Ppo Plans Dental Assistant Study Dental Office Management Dental Office Manager
Design Patterns Explained Dependency Injection With Code Examples
What Is Telemetry How Telemetry Works Benefits And Tutorial

Dental Claim Form 8 Reasons Why People Love Dental Claim Form Dental Medical Coding Teacher Templates

Coding And Reimbursement What Is Medical Necessity The American Academy Of Audiology

Coding And Reimbursement What Is Medical Necessity The American Academy Of Audiology

Doctors Tell All And It S Bad The Atlantic

The Case Against Breast Feeding The Atlantic

Why Doctors Hate Their Computers The New Yorker
Coding And Reimbursement What Is Medical Necessity The American Academy Of Audiology

What Are Category Iii Codes And How Are They Best Used For Billing

Dental Claim Form 8 Reasons Why People Love Dental Claim Form Dental Medical Coding Teacher Templates

What Is Medical Ethics And Why Is It Important
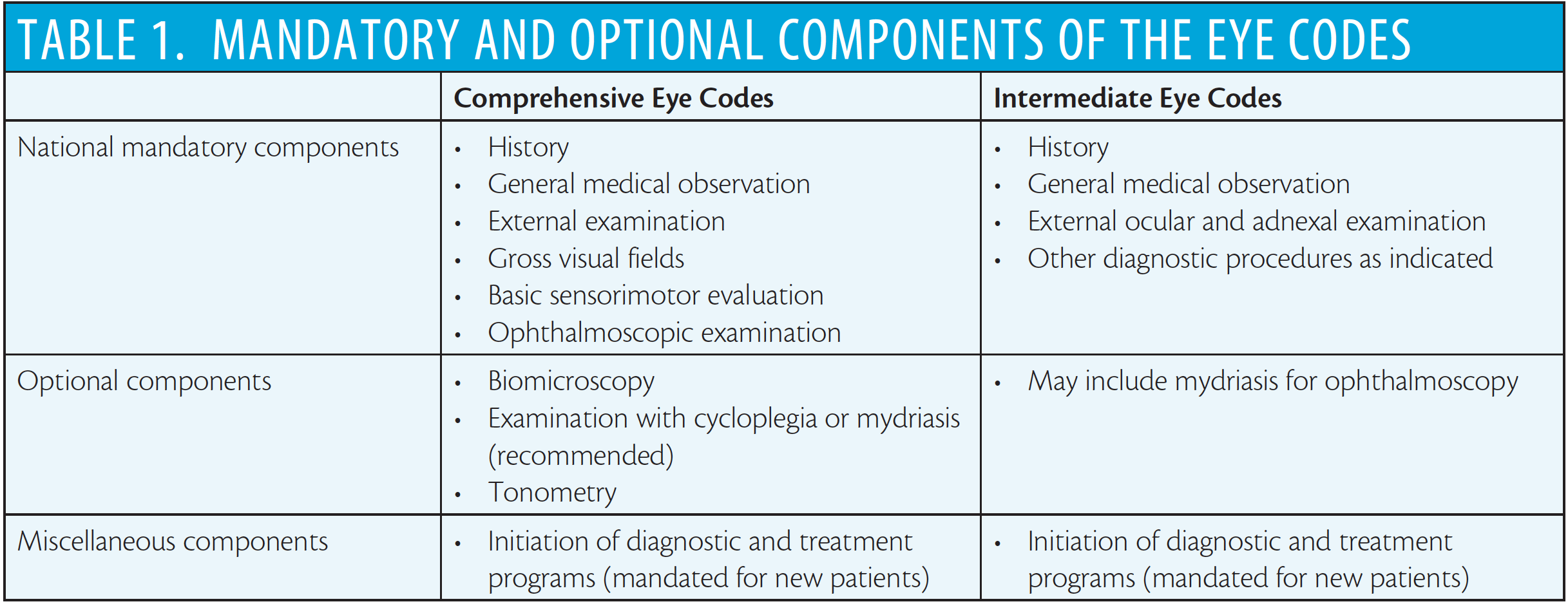
Perils Of The Eye Codes Retina Today

Submitting Dental Procedures To Medical Insurance Has Been Voodoo Until Now Dental Economics

Coding And Reimbursement What Is Medical Necessity The American Academy Of Audiology
/conceptual-image-of-geometric-blocks-1136585665-d4000c7c0ac84c02b77b672f9d2a3dcd.jpg)
Comments
Post a Comment